Sina Technology News Beijing time March 14 news, according to foreign media reports, to find the origin of depression, the average person will not think of the first time to study the patient's intestines. But as early as the early 20th century, a doctor named George Porter Phillips made this prediction.
While visiting the ward of the infamous "Insane House" at the Royal Hospital of Bethlehem, Phillips noted that people with depression often have serious constipation problems and other signs of "metabolism blocked", such as fragile nails and dull hair. , look pale and so on.
Most people think that depression is the cause of these physiological problems. But Phillips wondered if this causal arrow would just be reversed? If you are treating the intestines, can you alleviate depression? So he adjusted the patient's recipe and removed all the meat except the fish. He also allowed patients to drink milk-fermented beverages containing lactic acid bacteria to improve digestion with this probiotic.
Surprisingly, this method really worked. Of the 18 patients tested by Phillips, 11 had a complete cure for depression and two had significantly improved symptoms. This is the first to provide evidence that the gut flora can greatly affect mental health.
The BBC's "Microorganisms and Me" series of sciences has analyzed a number of arguments about the goodness of the gut flora, but it may be most unbelievable to say that they may be related to mental health. How do these micro-scavengers that feed on digestive tract residues affect our brains?
As mentioned in other articles in the series, some of these findings may be overstated and sensational. But the experiment from Phillips has been more than a century, and now the view of the "intestine-brain" theory has been deeply rooted in the hearts of the people. “Microbes can affect mental health, which seems to me to be unquestionable.†Jane Allyson Foster of McMaster University in Canada said her lab is the leader in the field. military. This means that we may be able to start from the abdomen and heal the brain. “This has great potential for new therapies and precision medicine.â€
Foster stressed that an unhealthy intestine is only one of the many causes of mental illness, so this new "psychology" therapy is only effective for a specific class of patients. But for patients suffering from imbalances in the gut flora, these new therapies may give them a long-lasting drought.
Although there were early studies conducted by Phillips et al., the idea that the intestines may affect mental health for most of the 20th century has not been favored by the academic community. It was not until the past 20 years that people found strong evidence to support this mysterious connection. The most striking experiment was carried out by Kyushu University in Japan in 2004. The team first verified that "sterile" mice (grown in a sterile environment, ensuring that there are no microbes in the body) have greater fluctuations in corticosterone and adrenocorticotropic hormone, both of which affect stress levels. This suggests that the intestinal flora of healthy mice can affect hormone levels in the body by some means.
Next, the researchers fed a group of sterile mice with lactic acid bacteria. Although the pressure response of these mice is still relatively large compared to mice that have not been cultured aseptically, it has been significantly reduced compared to mice without gut microbiota, and there are even signs that depression can be passed through the intestines. The flora is transmitted across species, such as from humans to mice.
In one study, researchers in Chongqing extracted a sample of intestinal flora from patients with major depression and implanted them into sterile mice. They then forced the mice to complete the "swim mission," and the mice that were implanted in the flora always gave up "outs" early. This behavior is like depression and lack of hope in patients with depression. The researchers then placed the mice in a box, and they seldom took the time to explore the middle part of the box, but instead gathered at the edges that made them feel safe.
“The most striking thing is that these small animals are able to accept the 'depressed' flora and then show depression,†said Julio Licinio, co-author of the paper and medical university in Northern New York. If you change the flora, you can change their performance."
We can only get these conclusions from these animal studies, but these conclusions are supported by large-scale epidemiological studies (the latest of which was published on February 4, 2019). These studies have shown that changes in the intestinal flora occur at the same time as a variety of mental illnesses, including depression and anxiety.
These effects are not caused by a single bacterium. On the contrary, the overall proportion of various bacteria seems to be the key. The diversity of intestinal flora in patients with depression and anxiety is smaller than that without mental illness. Surprisingly, a recent paper in Riccione pointed out that schizophrenia is associated with too little intestinal bacteria. The implantation of a sample of the intestinal flora of a patient with schizophrenia into a sterile mouse appears to have typical characteristics of the mental disorder in the brain activity of the mouse.
Multiple paths
 Among patients taking antidepressants, only 2 out of every 10 people showed signs of improvement.
Among patients taking antidepressants, only 2 out of every 10 people showed signs of improvement. These effects can be caused by multiple paths.
Some types of gut microbes protect the intestinal mucosa and prevent intestinal contents from entering the bloodstream. Without this barrier, you will get a "cold leak" that stimulates the release of pro-inflammatory cytokines. This protein increases the blood flow around the infection and regulates the body's immune response.
Although this response is essential for combating infection, cytokines can also cause depression and depression. This is why we often feel tired when we are sick. In the short term, this response can help us retain the energy to fight infection. But in the long run, it can lead to depression.
Intestinal microbes also affect our digestion and metabolism of important neurotransmitters such as dopamine. Our gut flora communicates directly with the brain, even through the vagus nerve. The vagus nerve is located near the inner layer of the intestine to check the body's digestive condition. Therefore, chemical "messengers" released by intestinal microbes can affect the signalling of the vagus nerve and thus alter brain activity. "In the gut, bacteria have many opportunities to 'communicate' with the host system, including the nervous system, etc." Foster said, "This is a very active, interactive and rich place."
However, these pathways are not “single lineâ€, so brain activity can also affect the composition of the gut flora. For example, stress can strengthen the inflammatory response, which in turn affects the intestinal flora. This result may form a type of "feedback loop."
New approach
 After transplanting a dose of "probiotics" into sterile mice, the researchers found that their stress response was significantly reduced.
After transplanting a dose of "probiotics" into sterile mice, the researchers found that their stress response was significantly reduced. Foster said that research in this field is developing rapidly. University scientists and commercial companies are all involved in the research. The meeting to discuss the results of the study "opens several times a week", which is no longer rare, and the researchers hope Their research can provide new treatments for diseases such as depression.
Current antidepressants are designed to regulate the balance of chemicals such as serotonin in the brain, but not for all patients. Among the patients taking the drug, only 2 out of every 10 people showed signs of improvement. Although this can help a lot of patients, the effects of language therapy such as cognitive behavioral therapy are also not satisfactory. Therefore, many patients can't benefit from it and can only find the right treatment for themselves. The “intestinal-brain†theory presented in this article seems to be the most promising option.
Some methods (such as the experiment that Phillips conducted in 1910) allowed patients to take fermented beverages to provide bacteria and beneficial digested proteins to the intestines; or to allow patients to ingest a soluble fiber called “prebiotics†to encourage the intestines. Bacterial reproduction. However, these studies tend to be too small, the number of subjects is ambiguous, and the results are mixed. In some studies, these interventions have successfully alleviated the patient's symptoms; but in other trials, the efficacy is better than placebo. How many.
Foster said that this may be because those failed experiments did not target patients who could benefit most from such treatment. After all, depression has many causes. Although some of the patients may have depression or anxiety caused by intestinal flora disorder, the pathogenic factors of other people may be quite different. For the latter group of patients, probiotic beverages do not cause too much change in the condition.
To complicate the situation, each person's gut flora is unique, so any treatment for the gut flora should take these differences into account. In general, the composition of the gut flora of the two people is only about 10% overlap.
Therefore, Foster believes that we should look for a more sophisticated approach to match the treatment to the patient. "This is where the 'intestinal-brain' theory works in precision medicine." Foster said that they hope to "find the 'biological type' in patients with similar physiological conditions." For example, before determining treatment options, First test the patient's inflammation level is high or low and so on.
Riccinio is also cautious about future research and believes that future research can help us find treatments for the "intestinal-brain" theory. He pointed out that the serious side effects of antidepressants limit the development of new drug therapies, but this approach may circumvent these problems. “The object of treatment is not the brain,†he said. “So I think the side effects are much smaller.â€
Eat like an Italian
 The Mediterranean diet is rich in fruits and vegetables, healthy fats, and the proportion of processed foods is low, which has a significant positive impact on the human body.
The Mediterranean diet is rich in fruits and vegetables, healthy fats, and the proportion of processed foods is low, which has a significant positive impact on the human body. There is now growing evidence that healthy, balanced eating habits as a preventive measure can effectively reduce the risk of diseases such as depression. And our current understanding of the "intestinal-brain" theory has also played a role in "adding bricks and tiles".
Many studies have analyzed the “Mediterranean dietâ€. In general, such eating habits are rich in vegetables, fruits, nuts, seafood, unsaturated fatty acids, vegetable oils, etc., refined sugar, red meat and processed meat are less. (Of course, this is only a general summary. After all, the eating habits of different regions in southern Europe are also very different.) In a four-year study conducted in Spain, people who used traditional Mediterranean eating habits suffered from depression. The probability is only about half of the others.
“Data showing the importance of nutrients to mental and brain health is now everywhere and highly consistent,†said Felice Jacka, a nutrition psychiatrist at Deakin University in Australia. Although there are many possible mechanisms, Mediterranean eating habits can indeed increase the diversity of the intestinal flora, and can also alleviate the physiological changes that often occur with depression, such as chronic inflammation.
It’s been more than a century since Phillips’ experiment at the Royal Hospital in Bethlehem, and the “Wanjin Medicine†for treating depression is still out of reach. But for at least some patients, a healthy bowel may be the first step to regain happiness. (leaf)
Source: Sina Technology
New product of U85 micro laser distance sensors use highly focused class 2 laser to detect objects or measure distances, and can return a measured value via varieties intface( serial, usb, rs232, rs485, bluetooth etc.). The electronic distance sensor is a very small Laser Distance Sensor, but high resolution up to 1mm and long distance measuring sensor - teachable measuring range of up to 30m. Extremely accurate distance sensing sensors, errors down to ± 1mm. And the mini sensors and measurements support continuous measurement function, great for compact solutions(eg: robots) with the smallest Laser Distance Sensor of the world!
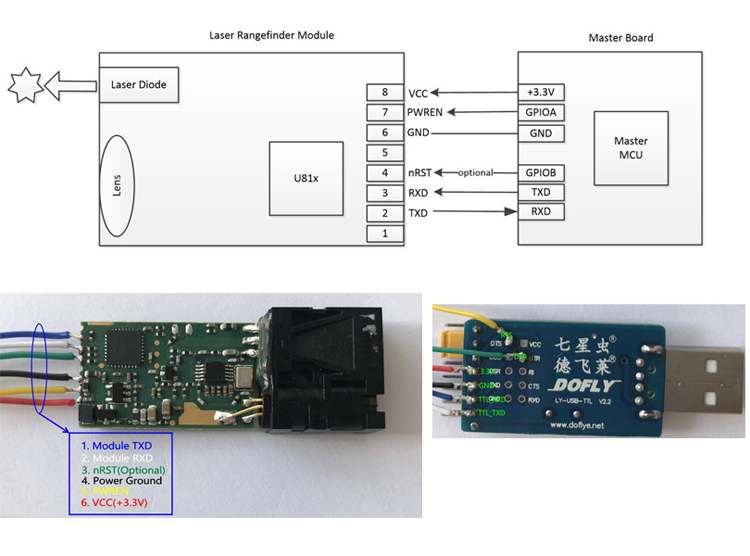
Parameters of U85:
Accuracy
±1 mm (0.04 inch)
Measuring Unit
mm
Measuring Range (without Reflection)
0.03-20m/0.03-30m
Measuring Time
0.1~3 seconds
Laser Class
Class II
Laser Type
620nm-690nm, <1mW
Size
41*17*7mm (±1 mm)
Weight
About 4g
Voltage
DC2.0~3V
Electrical Level
TTL/CMOS
Certifications
CTNT, FDA, CE, FCC, RoHS, etc.
Operating Temperature
0-40 ℃ (32-104 ℉ )
Storage Temperature
-25~60 ℃ (-13~140 ℉)
Mini Laser Distance Sensor,Optical Laser Distance Sensor,Smallest Laser Range Sonsor,Laser Measuring Sensor
Chengdu JRT Meter Technology Co., Ltd , http://www.rangesensors.com